true or false? individuals with bulimia nervosa are at risk for refeeding syndrome.
 Midterm.docx - Question 1 1 1 pts True or False Foods and beverages that provide vitamins minerals and other substances that contribute to adequate | Course Hero
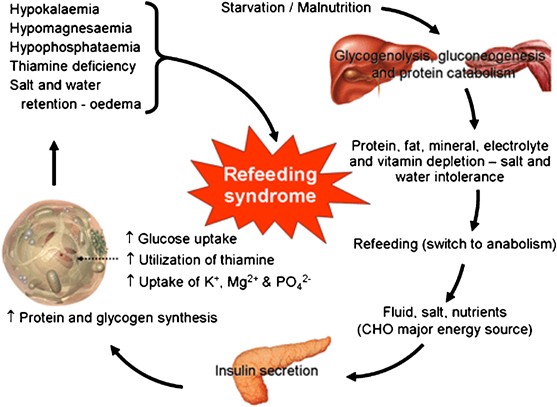
Midterm.docx - Question 1 1 1 pts True or False Foods and beverages that provide vitamins minerals and other substances that contribute to adequate | Course HeroWarning: The NCBI website requires JavaScript to operate. Reference Syndrome: what it is, and how to prevent and treat itHisham M Mehanna1Institute for Studies and Education of Heads and necks, Department of Otorhinolarynology—Cirugía de Carga y Cuello, Hospital Universitario, Coventry CV2 2DX 2Corazón de la Fundación England, Birmingham Jamil Moledina3Department of Otorhinolaryngology No randomized controlled treatment trials have been published, although there are guidelines that use better evidence available to manage the condition. In 2006 the National Institute of Health and Clinical Excellence (NICE) published a guideline in England and Wales. However, because doctors are often unaware of the problem, refeeding syndrome still occurs. This review aims to raise awareness of refeeding syndrome and discuss prevention and treatment. The available literature mainly includes weaker evidence (level 3 and 4), such as cohort studies, case series and consensus expert opinions. Our article also draws attention to the NICE guidelines on nutritional support in adults, with particular reference to new recommendations for best practice in refeeding syndrome. These recommendations differ in parts, and we believe that they improve the previous guidelines, such as those of the Parenteral and Enteral Nutrition Group of the British Dietary Association (box 1). Box 1 Why use the NICE guidelines on refeeding syndrome? The guidelines are the most recent complete review of the literature on refeeding syndrome The guideline development group was strongly multidisciplinary with extensive consultations with professional stakeholders and patients The guidelines clearly identify points of good practice and areas for further research The new guidelines offer explicit clinical criteria for patients "at risk" and "high risk" of developing refeeding syndrome, which allows for better identification and preventionFor patients with electrolyte deficits, the new guidelines recommend the immediate initiation of nutritional support at a lower rate, rather than waiting until the electrolyte imbalance has been corrected (as recommended in the previous guidelines), thus avoiding further nutritional deterioration in the patients refeeding is the problem of the problem of the disease. Referral syndrome can be defined as life-threatening changes in fluids and electrolytes that can occur in malnourished patients who receive artificial refeeding (either indoors or parenteral). These changes result from hormonal and metabolic changes and can cause serious clinical complications. The distinctive biochemical characteristic of refeeding syndrome is hypophosphataemia. However, the syndrome is complex and may also have abnormal balance of sodium and fluid; changes in glucose, proteins and fat metabolism; thiamine deficiency; hypokalaemia; and hypomagnesemia. How common is refeeding syndrome? The true incidence of refeeding syndrome is unknown, due in part to the lack of a universally accepted definition. In a study of 10 197 patients hospitalized, the incidence of severe hypophosphataemia was 0.43%, with malnutrition being one of the strongest risk factors. Studies report a 100% incidence of hypophosphataemia in patients receiving total parenteral nutrition solutions that do not contain phosphorus. When phosphate-containing solutions are used, the incidence can decrease to 18%. Several prospective and retrospective studies of hyperfood cohorts in intensive care units have documented the appearance of refeeding syndrome. In a prospective study of well-designed cohorts of a heterogeneous group of patients in intensive care units, 34% of patients experienced hypophosphataemia shortly after eating (mean (standard deviation) 1.9 (1.1) days). Many case reports have highlighted the potentially fatal nature of the condition. However, it is often not recognized or perhaps treated inappropriately, especially in the general chambers. How does refeeding syndrome develop? Protracted fast The underlying causative factor of refeeding syndrome is metabolic and hormonal changes caused by rapid refeeding, either intertwined or parenteral. The net result of metabolic and hormonal changes in early starvation is that the body changes from using carbohydrates to use fat and protein as the main source of energy, and the basal metabolic rate decreases by up to 20-25%. During prolonged fasting, hormonal and metabolic changes are aimed at preventing the breakdown of proteins and muscles. Muscle and other tissues diminish their use of ketone bodies and use fatty acids as the main source of energy. This leads to an increase in blood levels of the cetone bodies, stimulating the brain to change glucose to the cetone bodies as their main source of energy. The liver decreases its rate of gluconeogenesis, thus preserving muscle protein. During the period of prolonged starvation, several intracellular minerals are severely depleted. However, serum concentrations of these minerals (including phosphate) may remain normal. This is because these minerals are mainly in the intracellular compartment, which is contracted during the starvation. In addition, there is a reduction in renal excretion. RefeedingDuring refeeding, glucemia leads to greater insulin and a lower secretion of glucago. Insulin stimulates the synthesis of glucogen, fat and protein. This process requires minerals such as phosphate and magnesium and cofactors such as thiamine. Insulin stimulates the absorption of potassium in cells through the ATPase sodium-potassium simper, which also carries glucose in cells. Magnesium and phosphate are also taken in cells. Water is still for osmosis. These processes cause a decrease in phosphate, potassium and magnesium levels, all of which are already exhausted. The clinical characteristics of refeeding syndrome occur as a result of the functional deficits of these electrolytes and the rapid change in the basal metabolic rate. What electrolytes and minerals are involved in pathogenesis? Phosphorus is predominantly an intracellular mineral. It is essential for all intracellular processes and for the structural integrity of cell membranes. In addition, many enzymes and second messengers are activated by phosphate binding. It is important that it is also necessary for the storage of energy in the form of adenosine triphosphate (ATP). It regulates the affinity of haemoglobin for oxygen and thus regulates the delivery of oxygen to tissues. It is also important in the renal acid-based damping system. In refeeding syndrome, chronic depletion of the entire phosphorus body occurs. In addition, increased insulin causes the absorption and use of phosphate in cells. These changes lead to an intracellular and extracellular phosphorus deficit. In this environment, even small decreases in serum phosphorus can lead to widespread dysfunction in cell processes that affect almost every physiological system (see table A in bmj.com). PotassiumPotassium, the main intracellular cation, is also exhausted in malnutrition. Once again, the serum concentration can remain normal. With the change to anabolism in restitution, potassium is taken in cells as they increase in volume and number and as a direct result of insulin secretion. This results in severe hypokalaemia. This causes detachments in the electrochemical membrane potential, resulting in, for example, arrhythmias and cardiac arrest. MagnesiumMagnesium, another predominantly intracellular cation, is an important cofactor in most enzyme systems, including oxidative phosphorylation and ATP production. It is also necessary for the structural integrity of DNA, RNA and ribosomes. In addition, it affects the membrane potential, and deficiency can lead to heart dysfunction and neuromuscular complications. GlucoseGlucose intake after a period of starvation suppresses gluconeogenesis through insulin release. Thus, excessive administration can lead to hyperglycemia and osmotic diuresis sequel, dehydration, metabolic acidosis and cetoacidosis. Excessive glucose also leads to lipogenesis (again as a result of insulin stimulation), which can cause fatty liver, increased production of carbon dioxide, hypercapnea and respiratory insufficiency. Vitamin deficiency Although all vitamin deficiencies can occur at varying rates with inadequate ingestion, thiamin is of the greatest importance in refeeding complications. Tiamine is an essential coenzyme in carbohydrate metabolism. Its deficiency results in Wernicke's encephalopathy (ocular abnormalities, ataxia, state confusion, hypothermia, coma) or Korsakoff syndrome (retrograde and anterograted amnesia, confabulation). Sodium, nitrogen and liquid Changes in carbohydrate metabolism have a profound effect on sodium and water balance. The introduction of carbohydrate to a diet leads to a rapid decrease in sodium and water renal excretion. If fluid depletion is instituted to maintain a normal urine output, patients can quickly develop fluid overload. This can lead to congestive heart failure, pulmonary edema and cardiac arrhythmia. How can refeeding syndrome be prevented? The identification of high-risk patients is crucial (tables 2 and 3). Any patient with insignificant food consumption for more than five days is at risk of developing resentment problems. Patients may be malnourished as a result of a decrease in intake (e.g., due to dysphagia, nervosa anorexia, depression, alcoholism); reduction in the absorption of nutrition (e.g., inflammatory bowel disease, celiac disease); or increased metabolic demands (e.g. in cancer, surgery). High-risk patients are those who have been chronically malnourished, especially those who have also decreased the physiological reserve. Patients with dysphagia (e.g. as a result of a stroke) in particular may be at high risk. Box 2 Patients with high risk of refeeding syndrome Patients with Nervous anorexia Patients with chronic alcoholism Postoperative patients Older patients (comorbidities, decreased physiological reserve)Patients with uncontrolled diabetes mellitus (deplete electrolytes, diuresis)Patients with chronic malnutrition Or the patient has one or more of the following: Body mass index (kg/m2) Involuntary weight loss ±15% in the last three to six months Small or no nutritional intake for Â10 days Low potassium, phosphate or magnesium levels before feeding Or the patient has two or more of the following: Body mass index Unintentional weight loss 10% in the last three to six months Small or no nutritional intake for days History of alcohol or drug abuse, including insulin, chemotherapy, antiacids or diuretics The figure summarizes how to prevent and treat refeeding syndrome. In order to ensure proper prevention, the NICE guidelines recommend comprehensive nutritional assessment before restitution is initiated. Recent weight change should be determined with time, nutrition, alcohol intake and social and psychological problems. Plasma electrolytes (especially phosphate, sodium, potassium and magnesium) and glucose should be measured on the basis before feeding and correcting any deficiencies during feeding with close control. Management guidelines. Adapted from the guidelines of the NICE and the British Association of Parenteral and Enteral NutritionThe guidelines of the NICE recommend that resentment begin at no more than 50% of the energy requirements in "patients who have eaten little or nothing for more than 5 days". The rate can be increased if resentment problems are not detected in clinical and biochemical monitoring (recommendation level D-ver box 3). For patients with high risk of developing refeeding syndrome, the nutritional replenishment of energy should start slowly (maximum 0.042 MJ/kg/24 hours) and should be adapted to each patient. It can be increased to meet or exceed the full needs for four to seven days. In patients who are very malnourished (body mass index ≤14 or insignificant intake for two weeks or more), the NICE guidelines recommend that intake begin at a maximum of 0.021 MJ/kg/24 hours, with heart monitoring due to the risk of heart arrhythmias (level D recommendation). This explicit specification of the resentment rate in severely undernourished patients should help avoid complications arising from rapid refeeding and is an improvement in the previous guidelines. The NICE guidelines also indicate that it is not necessary to correct the electrolyte and liquid imbalances before feeding and that this should be done together with the feeding. This is a change in previous guidelines and potentially prevents the prolongation of malnutrition and its effects on patients. All guidelines recommend that supplementation of vitamins be initiated immediately, before and during the first 10 days of refeeding. The circulatory volume must also be restored. Oral, intrusive or intravenous supplements of potassium, phosphate, calcium and magnesium should be given unless the blood levels are high before refeeding. However, there are no good quality studies on the exact levels of supplementation, and therefore the required levels of these supplements cited by the NICE (Figure) are only level-D recommendations. Electrolyte levels should be measured once a day for a week, and at least three times in the following week. Urinary electrolytes could also be revised to help assess body losses and orient replacement. How can refeeding syndrome be detected and treated? Reference syndrome is detected considering the possibility of its existence and using the simple biochemical research described above. If the syndrome is detected, the feeding rate should be slowed and the essential electrolytes should be replaced. The specialist hospital diet team must participate. The best method for electrolyte replacement has not yet been determined. Hypophosphataemia, hypomagnesemia and hypokalaemia in hospitalized patients are ideally treated with intravenous supplementation (Table), but this is not without risk. A prospective study of comparative cohorts of 27 patients with severe hypophosphataemia showed the safety of administering phosphate of 15-30 mmol for three hours through a central venous catheter in an intensive care unit. However, researchers reported the need for repeated doses in most patients. Terlevich et al reported efficacy of 50 mmol phosphate infused in a peripheral vein for 24 hours in 30 patients without pre-existing kidney dysfunction in the general rooms. More infusions may be required and careful follow-up of blood levels is required. Care is needed in patients with existing kidney deficiency, hypocalcaemia (which may worsen), or hypercalcaemia (which may result in metastatic calcification). Recommendation for phosphate supplementation and magnesium3 4 6 13 MineralDosePhosphate Maintenance requirement0.3-0.6 mmol/kg/day verbally Hippophosphataemia mild (0.6-0.85 mmol/l)0.3-0.6 mmol/kg/day orally controlled Hypophosphataemia moderate (0.3-0.6 mmol/l) Sodium management should be limited to the replacement of losses. In patients with high risk of heart decompensation, central venous pressure and heart rate control should be considered. Conclusion Accession to the NICE guidelines to prevent and treat refeeding syndrome (tables 2 and 3) should reduce the incidence and associated complications of the syndrome. Further research is needed to determine the true incidence of refeeding syndrome and to determine the best management protocols. Abstract s Referral syndrome is a life-threatening condition, caused by the rapid initiation of restitution after a period of malnutrition It is characterized by hypophosphataemia, associated with fluid and electrolyte changes and metabolic and clinical complications The awareness of refeeding syndrome and the identification of at-risk patients is crucial, as the condition is preventable and metabolic complications are avoidable.High-risk patients include chronically undernourished patients and those who have had little or no energy intake for more than 10 daysFood should begin at a low level of energy substitution. Supplementing vitamins should also begin with refeeding and continue for at least 10 daysThe correction of the imbalances of electrolytes and liquids before the food is not necessary; it must be done together with the food criteria We use the terms "recommend", "syndrome", and "hypophosphataemia" to search for the databases Medline, Embase, ally CINE, Coch We evaluate the 151 documents identified for their relevance. We evaluate the quality of the evidence in the original articles according to the guidelines published on the Tests-Based On-Call website. Areas for future research Formulation of consensus definitions and results for nutrition reporting studiesInstant multicenter studies focused on homogeneous and well-defined study samples High-quality tests to identify the best replacement and treatment regimes for phosphate and other minerals for refeeding syndrome Complementary materialsNotesAn extra web box (box A) on the complications of refeeding syndrome is underlying. We thank Chuka Nwokolo (Department of Gastroenterology, Hospital Universitario, Coventry) for their efforts and comments to review this article. Collaborators: HMM planned the article, did the searches, evaluated the evidence, and wrote and revised the manuscript; he is also the guarantor. JM did the searches, evaluated the evidence, and helped with the article's writing. JT did the searches, evaluated the evidence, and revised the manuscript. Competing interests: None declared. Bear testing and peer review: Recommendations derived from low-grade testing — primarily cohorts and case series studies — and consensual expert opinion Footnotes*Recommendations derived from low-grade testing — mainly cohorts and case series studies — and expert consensus opinionReferencesFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA

Midterm.docx - Question 1 1 1 pts True or False Foods and beverages that provide vitamins minerals and other substances that contribute to adequate | Course Hero

Midterm.docx - Question 1 1 1 pts True or False Foods and beverages that provide vitamins minerals and other substances that contribute to adequate | Course Hero
Agenda True or False? True or False? True or False True or False

Midterm.docx - Question 1 1 1 pts True or False Foods and beverages that provide vitamins minerals and other substances that contribute to adequate | Course Hero
Agenda True or False? True or False? True or False True or False
Atypical early-onset eating disorders | Advances in Psychiatric Treatment | Cambridge Core
/refeeding-overview-4177196-FINAL-bc7de67dc8ae4789abdf5d735b4fef45.png)
An Overview of Refeeding Syndrome

The Disconnected Self: Assessment and Treatment of Eating Disorders - ppt download

The Disconnected Self: Assessment and Treatment of Eating Disorders - ppt download

Academy of Nutrition and Dietetics: Revised 2020 Standards of Practice and Standards of Professional Performance for Registered Dietitian Nutritionists (Competent, Proficient, and Expert) in Eating Disorders - Journal of the Academy of

Practice-Based Evidence and Clinical Guidance to Support Accelerated Re-Nutrition of Patients With Anorexia Nervosa - Journal of the American Academy of Child & Adolescent Psychiatry
PDF) Practical methods for refeeding patients with anorexia nervosa
Identification and Treatment of Eating Disorders in the Primary Care Setting

Hypophosphataemia in anorexia nervosa | Postgraduate Medical Journal
CSW Eating Disorder - Refeeding Pathway

Anorexia Nervosa and Bulimia Nervosa - Pediatrics House Staff

PDF) Legal and Ethical Issues in the Treatment of Really Sick Patients with Anorexia Nervosa
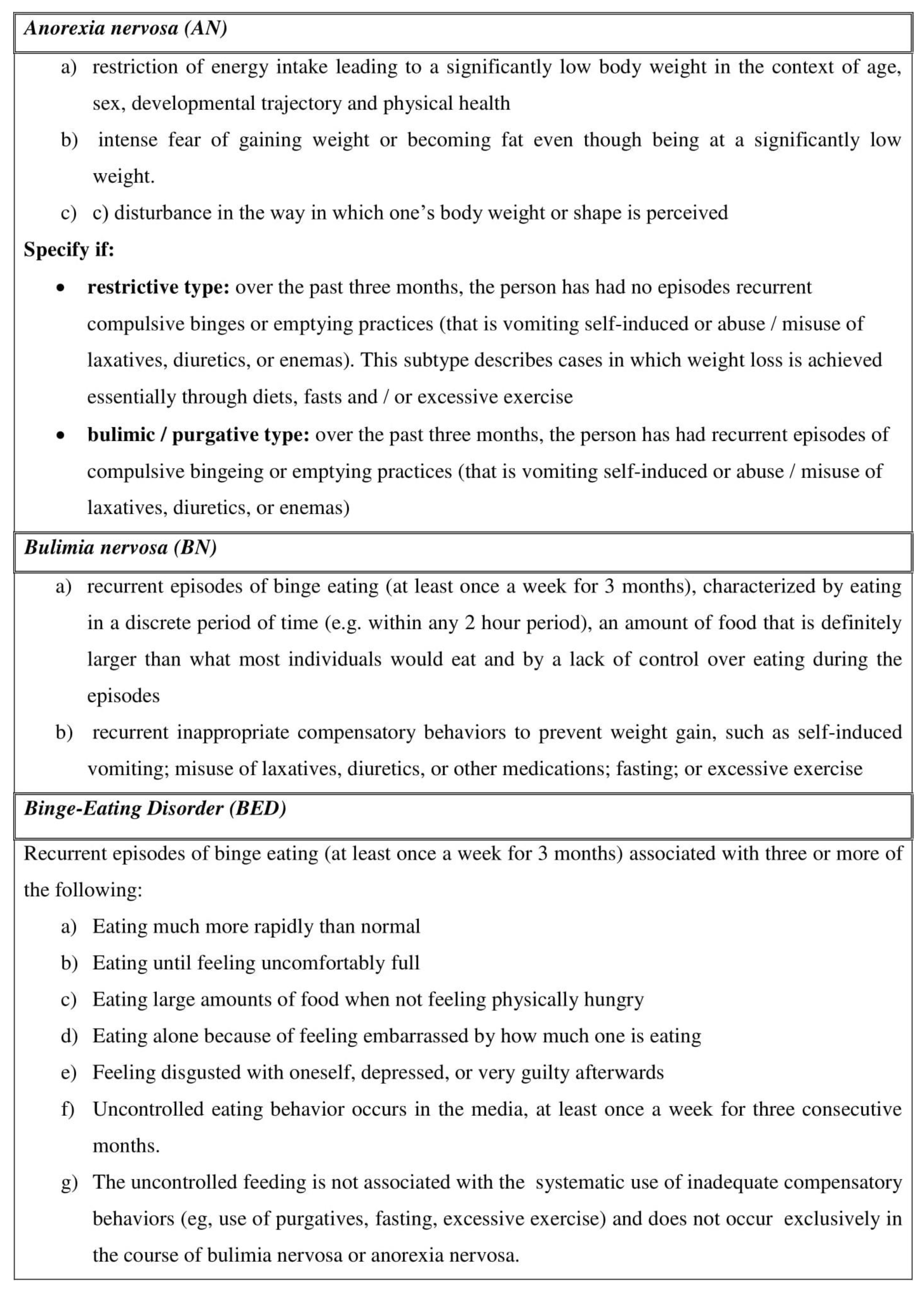
Eating Disorders' Assessment and MNT.doc

realimentacion uptodate | Heart Failure | Anorexia Nervosa
Assessment and management of eating disorders: an update
Diagnosis and clinical features (Section 3) - Medical Management of Eating Disorders
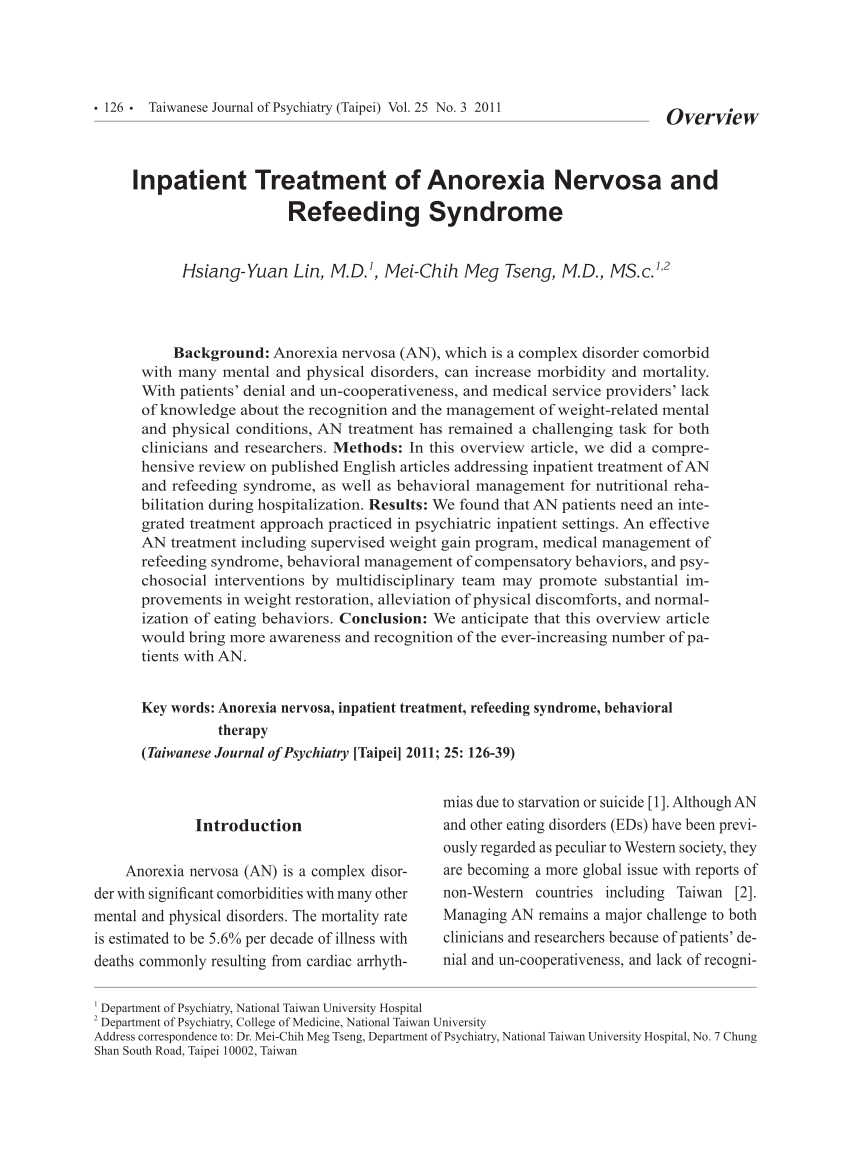
PDF) Inpatient Treatment of Anorexia Nervosa and Refeeding Syndrome

Genetics of eating disorders in the genome-wide era | Psychological Medicine | Cambridge Core

Eating disorders in adolescents with chronic gastrointestinal and endocrine diseases - The Lancet Child & Adolescent Health
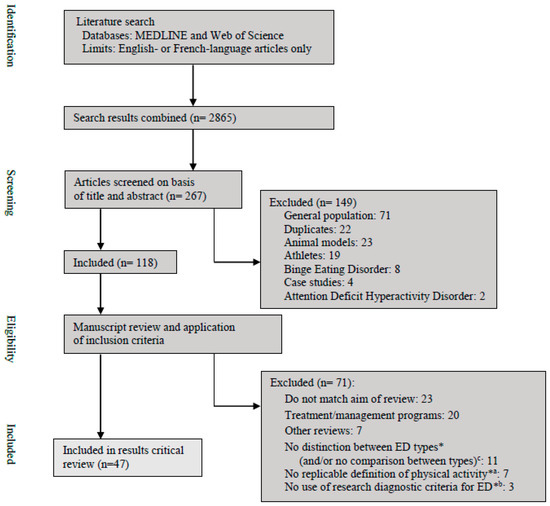
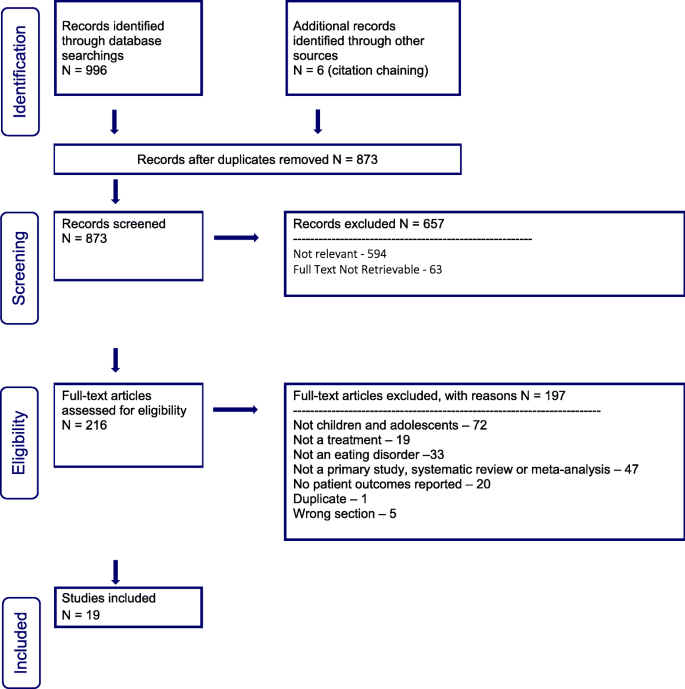
Nutrients | Free Full-Text | Physical Activity in Eating Disorders: A Systematic Review | HTML
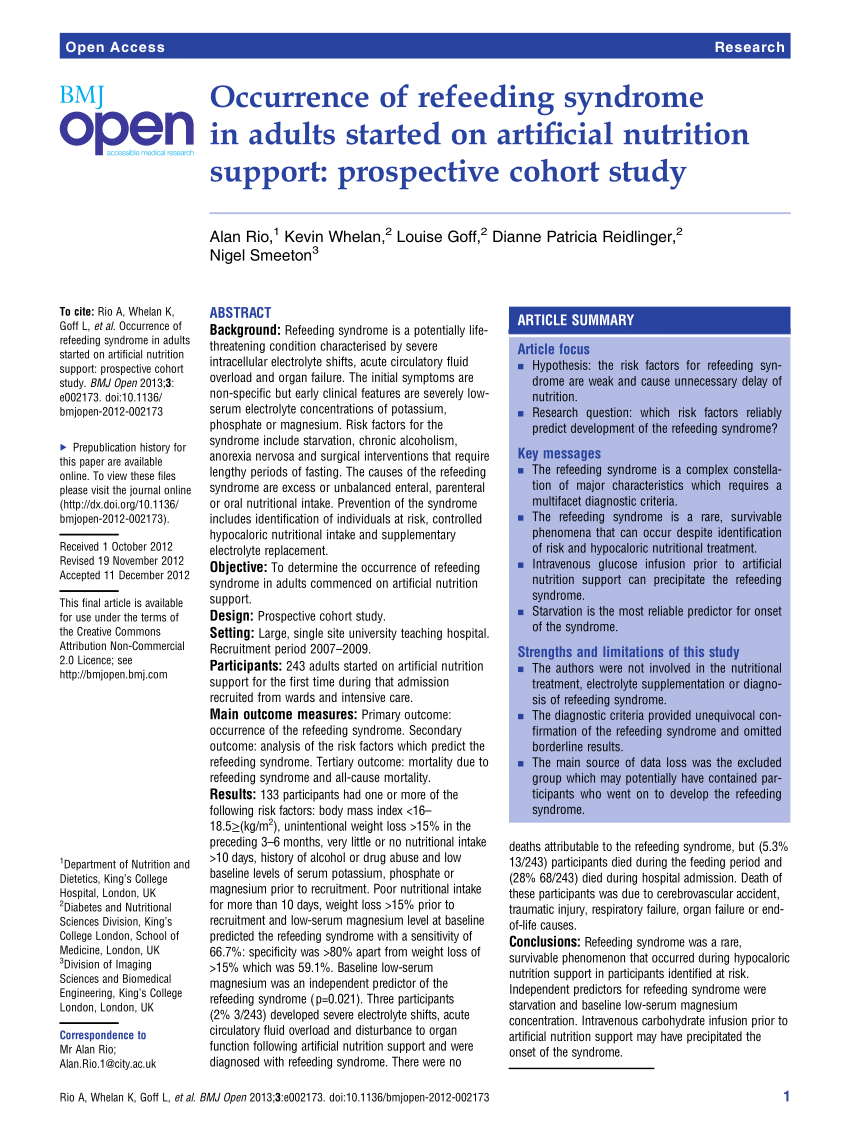
PDF) Occurrence of refeeding syndrome in adults started on artificial nutrition support: Prospective cohort study
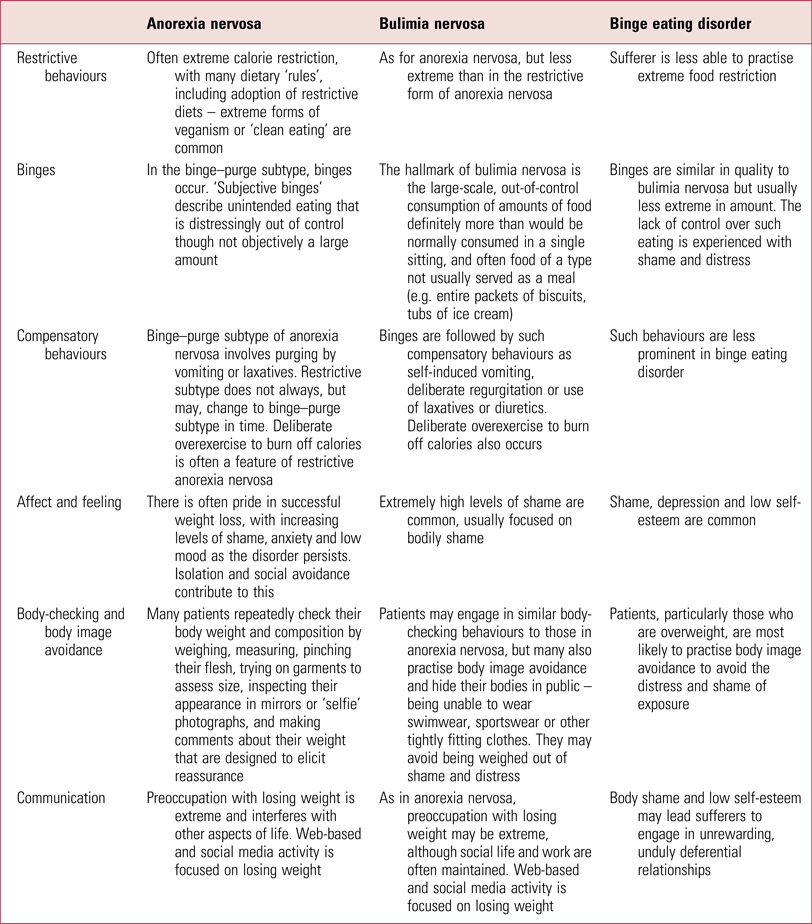
An update on eating disorders | BJPsych Advances | Cambridge Core

Position of the American Dietetic Association - Journal of the American Dietetic Association
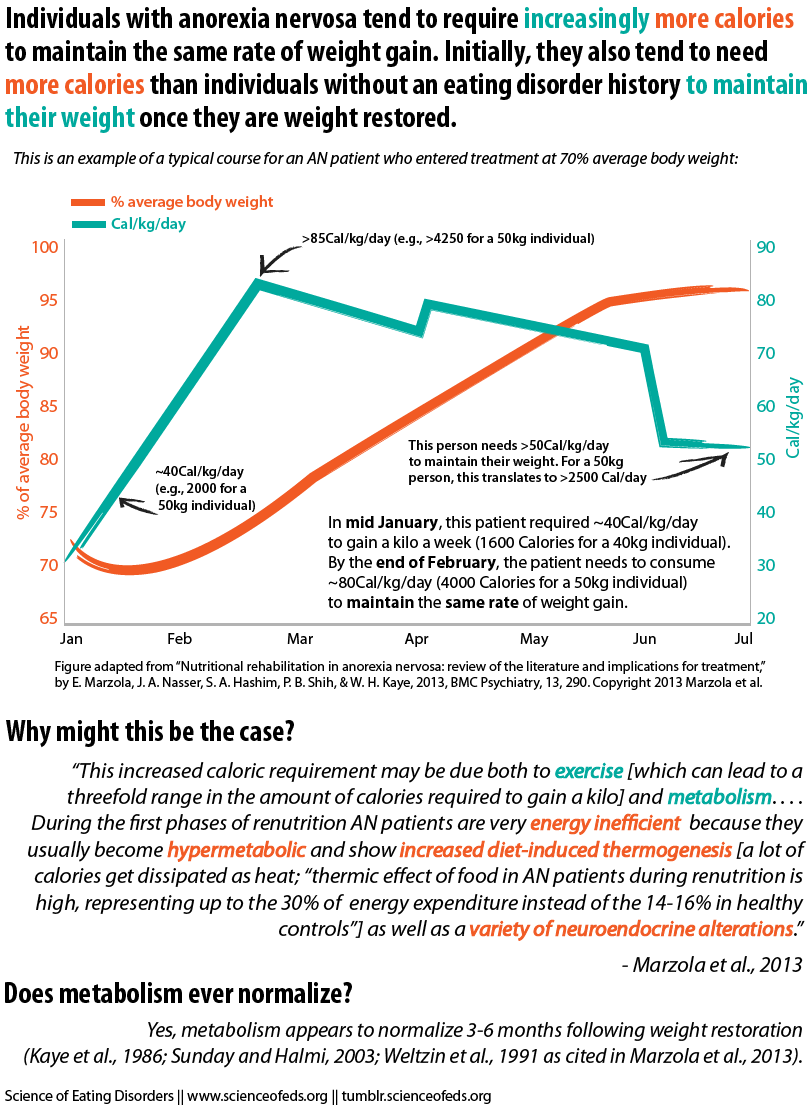
Hypermetabolism in Anorexia Nervosa – Science of Eating Disorders
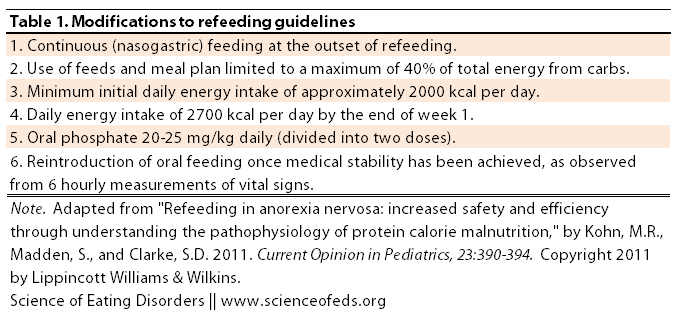
Avoiding Refeeding Syndrome in Anorexia Nervosa – Science of Eating Disorders
Eating disorders in children, adolescents, and young adults
Nutrients | Free Full-Text | Eating Disorders and Gastrointestinal Diseases | HTML
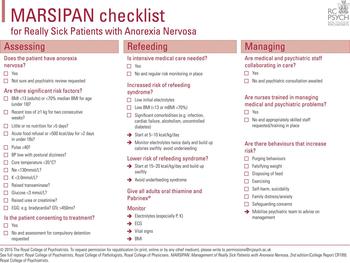
MARSIPAN: management of really sick patients with anorexia nervosa | BJPsych Advances | Cambridge Core

In Defense of Eating Junk Food in Eating Disorder Treatment – Science of Eating Disorders

NICE guidelines for identification of patients at high risk for... | Download Scientific Diagram

Eating disorders - The Lancet
Nutrition in clinical practice—the refeeding syndrome: illustrative cases and guidelines for prevention and treatment | European Journal of Clinical Nutrition
Canadian practice guidelines for the treatment of children and adolescents with eating disorders | Journal of Eating Disorders | Full Text
Eating Disorder and Mental Health: Anorexia Nervosa and Obsessive-Compulsive Disorder as Comorbidities Cindy Kang The Universit
Posting Komentar untuk "true or false? individuals with bulimia nervosa are at risk for refeeding syndrome."